
Triage is a critical aspect of nursing, particularly in high-stakes environments like emergency rooms, disaster response settings, and telemedicine. It involves prioritizing patient care based on the severity of their condition, ensuring that those with life-threatening issues receive immediate attention. As healthcare systems become increasingly complex and demands on nurses grow, understanding the principles, types, and challenges of triage is essential for efficient patient care.
The word "triage" originates from the French term "trier," meaning to sort. In healthcare, triage refers to the process of sorting and classifying patients based on the urgency of their medical condition. Triage is applicable across various healthcare settings to ensure that limited resources such as time, personnel, and medical supplies are utilized in the most effective way possible.
In nursing, triage requires quick and accurate assessments, critical thinking, and decision-making skills. Nurses trained in triage must rapidly assess a patient's symptoms, decide on the level of care they require, and act accordingly. The primary goal of triage in nursing is to identify and prioritize those who need immediate medical intervention, preventing delays that could result in adverse outcomes for the patient.
Triage assessment involves a series of systematic steps that enable healthcare professionals to categorize patients. These steps are crucial in managing patient flow, especially in crowded or high-pressure environments like emergency departments or during disasters.
The first step in a triage assessment is a quick, but thorough, visual assessment of the patient. Nurses assess factors such as skin color, respiratory effort, and overall demeanor to identify any obvious signs of distress. This quick glance can reveal life-threatening conditions like severe bleeding, respiratory distress, or unresponsiveness.
A more detailed assessment follows, known as the primary survey. This includes evaluating the patient's Airway, Breathing, Circulation, Disability (neurological status), and Exposure (known as the ABCDE assessment). During this stage, nurses check for clear airways, proper breathing patterns, adequate blood circulation, and neurological responses. The aim here is to identify and address life-threatening issues quickly.
Vital signs—such as heart rate, blood pressure, respiratory rate, and temperature—are then measured. This data provides valuable insight into the patient's condition and helps nurses determine the urgency of care. Abnormal vitals indicate a higher priority, especially when signs of life-threatening conditions are present.
Gathering subjective information from the patient is also essential. Nurses ask about the patient’s pain level, symptoms, medical history, and the onset of their current condition. The patient’s description of their symptoms is often a key component of the triage process, as it helps to differentiate between conditions of varying severity. Age, medical history, and potential risk factors are critical in the decision-making process. Patients with acute symptoms that indicate possible life-threatening conditions, like heart attacks or strokes, are prioritized. Likewise, elderly patients, infants, and those with chronic conditions (e.g., heart disease, asthma) may be seen sooner due to a higher risk of complications.
Once the nurse has collected all the data, the nurse classifies the patient into an appropriate triage category. This categorization is based on the urgency of the condition, and patients are assigned levels of priority—ranging from those who need immediate care to those who can safely wait.
Nurses may encounter several different types of triage that depend on the healthcare setting they are posted or working. Each type of triage has its own processes and challenges.
The most common form of triage, emergency room triage, involves assessing patients as they arrive in the ER. Nurses classify patients into categories based on how critical their condition is. Those with life-threatening injuries, such as heart attacks, strokes, or severe trauma, are seen first, while patients with less urgent conditions may wait longer. ER triage typically follows a five-level system like the Emergency Severity Index (ESI), which ranges from immediate resuscitation needs (Level 1) to non-urgent cases (Level 5).
Disaster triage is used in mass casualty situations, such as natural disasters, terrorist attacks, or major accidents. In these scenarios, the number of patients often overwhelms the available healthcare resources. The goal of disaster triage is to maximize the number of survivors by providing care to those most likely to benefit from immediate medical attention. A common disaster triage method is the START (Simple Triage and Rapid Treatment) system, which uses color codes to prioritize patients: red for immediate care, yellow for delayed care, green for minor injuries, and black for deceased or expectant.
Telephone triage is becoming more prevalent, especially with the rise of telemedicine. In this setting, nurses assess patients over the phone to determine whether they need immediate care, can wait to see a doctor, or should follow home-care instructions. Telephone triage requires excellent communication skills and the ability to gather accurate patient information without a physical examination.
Labor and delivery triage involves assessing pregnant women who come to the hospital to determine the stage of labor or whether there are any complications. Nurses evaluate factors such as contractions, fetal heart rate, and maternal vital signs to decide whether the patient should be admitted for delivery or further observation.
Pediatric triage requires specialized skills, as children often present differently from adults and may not communicate their symptoms effectively. In this type of triage, nurses assess a child's appearance, work of breathing, and circulation to the skin. Special attention is paid to signs like lethargy, irritability, or abnormal respiratory patterns.
Having looked at the types of triage, let us divulge into the common triage categories. Nursing students and nurses must understand triage categorization.
Triage categorization is the process by which patients are sorted and prioritized based on the severity of their condition and the urgency of their need for medical attention. This system ensures that those in the most critical conditions receive immediate care, while others may wait based on the relative seriousness of their medical issues.
Different triage systems and categories are used across healthcare settings such as emergency departments, disaster scenarios, and labor and delivery units. Each system follows specific guidelines and protocols to classify patients effectively.
Triage systems typically classify patients into distinct categories or levels, usually ranging from those needing immediate resuscitation to those with non-urgent conditions. Below are examples of common categorization methods used in triage.
In many emergency departments, five-level triage systems are the standard. These systems, such as the Emergency Severity Index (ESI) or the Canadian Triage and Acuity Scale (CTAS), help clinicians assess the urgency of patients' conditions based on both subjective and objective data, such as symptoms and vital signs.
This level is for patients with life-threatening conditions who need immediate care. Examples include cardiac arrest, major trauma, or severe respiratory distress. Without rapid intervention, these patients are at risk of death.
These patients also require immediate attention but are stable enough to allow for a slightly delayed response. Conditions in this category include severe chest pain (possible heart attack), stroke symptoms, or acute shortness of breath.
Patients at this level have conditions that are serious but not immediately life threatening. These include moderate to severe pain, high fever, or significant injuries such as fractures. Patients in this category should be treated within a short period but may wait a little longer than those in Level 1 or 2.
These patients have less severe symptoms and may wait for extended periods. Examples include minor injuries like sprains, cuts needing stitches, or a mild fever.
These patients have the lowest priority and can wait the longest for care. Common examples include routine medication refills, minor rashes, or mild cold symptoms. Their condition is stable and unlikely to worsen during the wait.
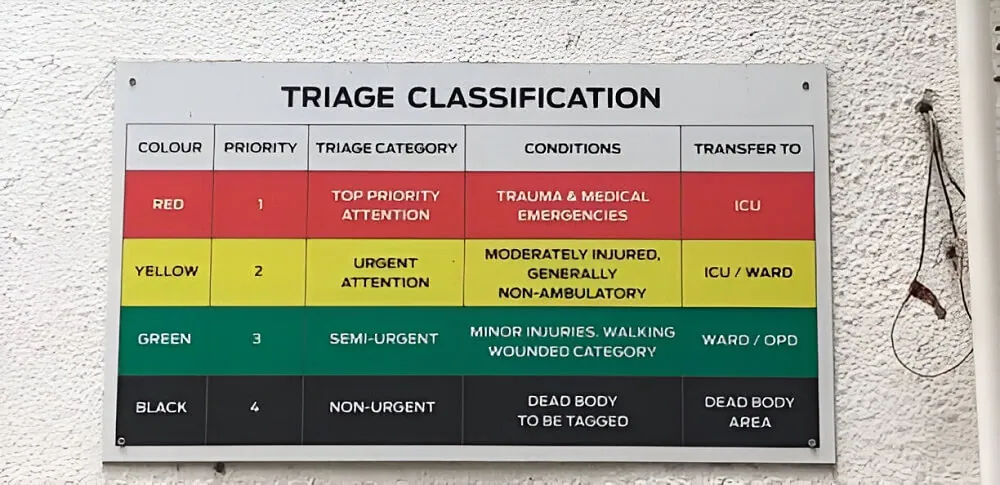
In disaster settings, where there are often mass casualties and limited resources, a color-coded system is frequently used to categorize patients quickly. One widely used system is the START (Simple Triage and Rapid Treatment) system, which assigns patients into four categories based on the severity of their injuries.
These patients have life-threatening injuries but are likely to survive with immediate treatment. Examples include severe bleeding, respiratory distress, or shock. Red-tagged patients are the highest priority in a disaster setting.
These patients have serious injuries that need medical attention but can wait without immediate danger. They are stable for the moment but require care eventually. Examples include fractures or wounds that need surgical intervention but are not life threatening.
Patients in this category have minor injuries that do not require immediate attention. They can typically walk or move on their own and can wait for treatment after patients that are more critical are treated. Examples include minor cuts, sprains, or abrasions. These patients are often referred to as "walking wounded."
These patients either are deceased or have injuries so severe that they are unlikely to survive, even with medical intervention. The focus in a disaster setting is to conserve resources for those who have a chance of survival. In cases where there are limited resources, these patients may not receive immediate care.
Below is an image representation.
In labor and delivery units, triage categorization focuses on assessing the stage of labor and identifying any complications that could endanger the mother or baby. Pregnant women presenting at the hospital are quickly assessed to determine whether they are in active labor, experiencing complications, or simply need observation.
This includes conditions such as placental abruption, fetal distress, or severe preeclampsia, which require immediate intervention to prevent harm to the mother or baby.
Cases where the patient is in active labor or presenting signs of labor (e.g., regular contractions and cervical dilation) without complications. The goal is to admit the patient for delivery.
Patients experiencing mild contractions, early signs of labor, or pre-labor symptoms but not in active labor are typically categorized as non-urgent. They may be observed over time or sent home with instructions.
In telehealth or telephone triage, nurses assess patients over the phone. The nurses determine whether they need immediate in-person care, can be seen later, or can manage their symptoms at home. Patients are often categorized based on the urgency of their symptoms.
Patients describing symptoms of severe chest pain, difficulty breathing, severe injuries, or stroke symptoms are immediately advised to seek emergency care.
These patients may not need emergency services but should see a healthcare provider on the same day. Examples include patients with a high fever, persistent vomiting, or moderate to severe pain.
Conditions that do not require urgent attention can be scheduled for a regular appointment. Examples include routine check-ups, medication refills, or mild, non-urgent symptoms.
Patients with minor issues such as mild cold symptoms, slight aches, or minor cuts may be advised to treat themselves at home using over-the-counter remedies and follow-up if symptoms worsen.
Several factors influence how patients are categorized during the triage process, including:
Related:
Triage nursing is governed by several core principles that guide the decision-making process.
Triage nurses face numerous ethical and moral dilemmas, as they must balance patient needs, resource limitations, and the urgency of each case. Key ethical considerations include:
Triage decisions must be fair and free of bias. Nurses aim to treat all patients with equal respect, regardless of race, socioeconomic status, or background. Ethical practice demands that personal characteristics not influence the prioritization of care. Triage inherently involves treating some patients before others, which can raise concerns about equality of care. While triage is based on medical necessity, there is always the risk that unconscious biases related to race, gender, or socioeconomic status may affect decision-making. It is essential that triage nurses are aware of these potential biases and actively work to ensure that all patients receive fair and equitable care.
One ethical challenge in triage is balancing patient autonomy with the nurse’s professional judgment. While patients have the right to autonomy in their care decisions, the triage process may limit their control over when they are seen. Patients may demand immediate care even if their condition does not warrant it, and nurses must make decisions that may conflict with the patient’s wishes. Ensuring that patients understand the rationale behind triage decisions can help mitigate this issue. Nurses must strive to explain triage protocols to manage expectations, balancing autonomy with the need for timely and organized care.
Beneficence (doing good) and non-maleficence (doing no harm) are core ethical principles guiding triage. Nurses prioritize patients based on the potential for immediate harm if care is delayed, ensuring that those with the most critical needs are attended to first.
In some triage settings, such as during a disaster or in a fast-paced emergency room, nurses may have to make quick decisions without obtaining full informed consent from the patient. This can lead to ethical concerns about whether patients are fully aware of the treatments they are receiving. In situations where consent is not possible, nurses must prioritize patient safety and well-being while striving to keep patients informed to the best of their ability.
When resources are limited, triage nurses may be forced to make difficult decisions about resource allocation. This can raise ethical questions about who should receive life-saving treatments when there are limited supplies or staff. In such cases, the principle of "the greatest good for the greatest number" often applies, but making these decisions can be emotionally and ethically challenging. Nurses may experience moral distress when they are unable to provide care to every patient in need due to resource constraints.
Triage decisions must also be legally sound. Triage nurses may face legal issues if a patient’s condition is misclassified or if there is a delay in treatment that leads to harm. Accurate documentation is critical to protecting nurses from liability, as it provides evidence of the rationale behind triage decisions. Nurses document assessments and decisions to ensure transparency, which can be critical if a patient’s condition worsens during a wait. This documentation protects both the patient’s rights and the nurse’s legal accountability.
Related Reading:
Despite the challenges, triage nursing offers numerous opportunities for growth, specialization, and professional development. As healthcare continues to evolve, the role of triage nurses becomes increasingly critical in ensuring patient safety and improving healthcare outcomes.
Triage nursing offers the opportunity to specialize in different areas, such as emergency, pediatric, or disaster nursing. Specializing allows nurses to develop expertise in a particular area and improve the quality of care they provide. Nurses with advanced training in triage are often highly sought after in emergency departments, disaster response teams, and urgent care centers.
With the rise of telemedicine, there is a growing demand for nurses trained in remote or telephone triage. This type of triage allows nurses to assess patients over the phone or through video consultations, helping to manage patient flow in clinics and emergency departments while ensuring patients receive appropriate care. The convenience of telehealth is particularly valuable in rural or underserved areas where access to healthcare is limited.
Experienced triage nurses can pursue leadership positions within their healthcare institutions, such as becoming a triage coordinator or clinical educator. In these roles, they can mentor new nurses, develop triage protocols, and improve the overall efficiency of the triage process. Additionally, experienced triage nurses may contribute to developing triage software or protocols that improve patient care.
There are opportunities for nurses to engage in research and innovation in triage nursing. Nurses can explore ways to improve triage accuracy, reduce wait times, and enhance patient outcomes. Research into how artificial intelligence (AI) and machine learning can assist in triage assessments is one area with significant potential. Nurses involved in research can contribute to evidence-based practices that improve patient care in both every day and disaster scenarios.
Triage nurses with experience in disaster nursing may find opportunities to work with international organizations such as the World Health Organization (WHO) or Doctors Without Borders. In these roles, nurses play a crucial part in disaster response and humanitarian efforts, providing care to populations affected by natural disasters, conflicts, or public health emergencies. This global work is not only fulfilling but also offers valuable experience in managing complex medical crises.
Triage nursing is not limited to hospitals or disaster zones. Community health centers, urgent care clinics, and even school health services are increasingly relying on triage nurses to assess patients quickly and direct them to the appropriate level of care. This shift represents an opportunity for triage nurses to impact public health at the community level, particularly in underserved areas.
Triage is a cornerstone of nursing practice in various healthcare settings, from emergency departments to disaster zones. It involves the rapid and accurate assessment of patients, allowing nurses to prioritize care based on the severity of the condition. Triage nursing is governed by principles that ensure patient care is delivered in the most efficient and equitable way possible, even in the face of limited resources.
While triage nursing comes with its own set of challenges—such as overcrowding, resource limitations, and ethical dilemmas—it also offers opportunities for specialization, leadership, and innovation. Nurses trained in triage play a vital role in improving patient outcomes, both in everyday clinical settings and during times of crisis.
As healthcare continues to evolve and the demand for skilled nurses grows, the role of triage nurses will become even more critical. By ensuring that the right care is delivered to the right patient at the right time, triage nurses help to optimize healthcare delivery, improve patient outcomes, and ensure that limited resources are used wisely.